Posted by Dr Sophie Bostock - Sleep Expert on 21st Oct 2022
How to Keep Cool and Sleep Well During Menopause
Sleep problems are very common for women going through menopause and can have a huge impact on quality of life.
Research suggests that more than half of women notice disrupted sleep during perimenopause. And for others, sleep problems can occur later, or post-menopause.
Sleep problems can resolve themselves, but as many as 1 in 4 women will experience insomnia during menopause. Insomnia disorder is a chronic sleep problem, defined as difficulty falling asleep, waking up repeatedly during the night or waking up feeling unrefreshed for at least 3 nights a week, for 3 months or more, which has a negative impact on daytime functioning.
What’s more, we all know just how hard to sleep it is when it’s hot and humid. We tend to fall asleep later, rise earlier, and sleep less overall in high temperatures. But it’s not only the outside temperature that can interfere with sleep. For many women, waking up with night sweats can have a devastating impact on sleep.
5 ways in which the menopause interferes with sleep
There are at least 5 reasons why menopause can interfere with sleep. Find out more below.
1. Hot flushes and night sweats
Hot flushes are a consequence of the hormonal changes happening during menopause. While not every hot flush will wake you up, they are linked to increased arousal in the brain, leading to lighter sleep. If you are woken up during the night, try not to get frustrated - you may not be able to prevent hot flushes from occurring, but you can make it easier to fall back to sleep.
Have a fan in the bedroom to help keep air circulating. You could also try sleeping on a towel, so that it’s easy to change if you wake up bathed in sweat. Focus on getting comfortable and allow yourself to relax. Cutting back on caffeine and alcohol can help some women to reduce hot flushes, as well as improving sleep quality. Find out more about sleep and night sweats during menopause and how to cope with them below.
2. Pain and inflammation
Recent studies point towards an increase in pain and inflammation during menopause, which can disrupt sleep. Ask your medical team about the right pain medication. Practicing mindfulness meditation has also been found to help with pain management.
3. Nocturnia, or waking up to have a wee during the night
Lower levels of oestrogen can lead to drying of the genital tract, discomfort and strong urges to urinate; which can disrupt sleep. Treating vaginal dryness can help with this. You might also want to keep a track of your fluid intake for a week or two, to see whether cutting back on fluids in the last hour before bedtime makes a difference.
4. Stress and low mood
Menopause often occurs at a time in women’s lives that is full of emotional challenges including an empty nest, caring for elderly parents, and career transitions. Volatile hormones make women more vulnerable to poor mental health. Lower levels of oestrogen can alter the regulation of hormones and transmitters which influence mood, such as serotonin. Stress is bad news for sleep, and lack of sleep can amplify the effects of stress. Fortunately, if you can get sleep under control, it can make everything else easier to cope with.
5. Higher rates of other sleep disorders, including sleep apnoea and restless leg syndrome
Sleep Apnoea, or OSA, is a condition where narrowing of the upper airways leads to pauses in breathing throughout night, and is often associated with snoring. OSA disrupts deep sleep and leads to extreme sleepiness during the day. Sleep apnoea can occur at any age but becomes more common in postmenopausal women. This is likely due to a reduction of the hormone progesterone.
In Restless Legs Syndrome (RLS), a sudden urge to move your legs interferes with getting to sleep. RLS seems to be more common in perimenopause, especially for women who have night sweats.
If you suspect that you’re suffering from a sleep disorder such as insomnia, OSA or RLS, and you’re having difficulty coping, speak to your doctor or healthcare team about evidence-based treatment.
Although sleep problems are very common, they are not inevitable. There are lots of things you can do to improve the quality of your sleep, regardless of what your hormones are up to.
So what causes night sweats during menopause, and what can we do about it?
Our sleep and body temperature are closely related. Every night as it gets dark, a steep drop in body temperature coincides with the release of the hormone melatonin, and these signals cue the body that it’s time to fall asleep.
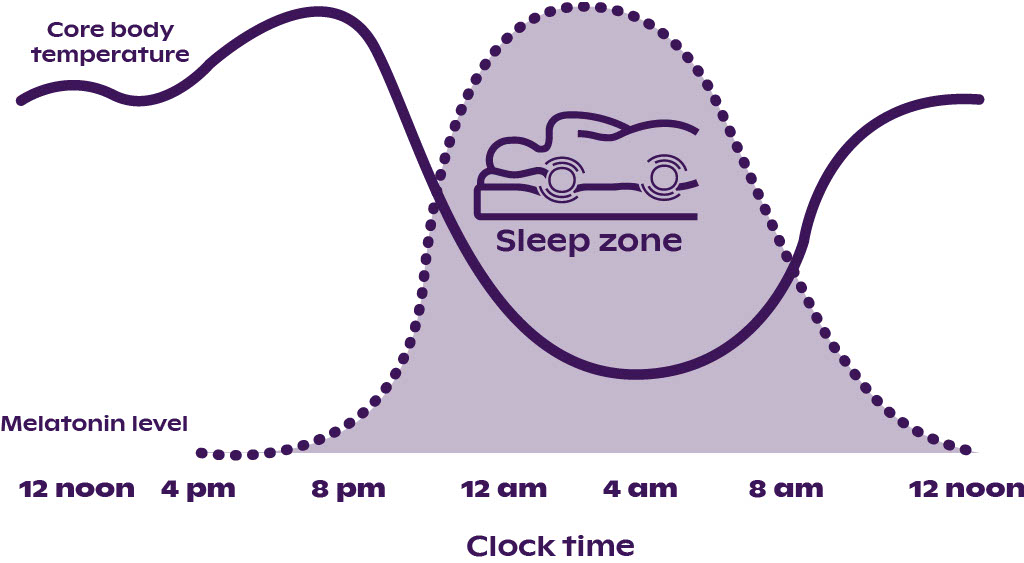
Fig. 1. The relationship between the circadian rhythms of core body temperature (solid line) and melatonin (dotted line) for a good sleeper who normally sleeps between 11:00 PM and 7:00 AM. Adapted from Lovato (2013).
This natural nightly drop in body temperature is usually achieved by sending more blood flow to the skin. As warm blood passes close to the thin blood vessels at the body’s surface, heat is transferred out to the colder air around us, and we cool down.
If our environment gets too hot, above about 25C, it’s much harder to cool down. Studies have found that being in a warmer environment interferes with both falling asleep and staying asleep. We tend to have less of the deep, slow wave sleep, which is very physically restorative. We also miss out on REM or rapid eye movement sleep, which is important for keeping us feeling balanced emotionally.
Why do we sometimes sweat at night?
If temperature varies by more than a few degrees, the brain brings more active heat regulation strategies into play. If we get too cold, we start to shiver so that the contraction of muscles releases heat energy. If we get too hot - for example through vigorous physical activity - our sweat glands release sweat, a combination of water and salts. The energy needed for beads of sweat to evaporate from the surface of our skin releases heat energy, and we cool down faster.
Interestingly, we can also sweat when we’re scared, nervous, or stressed. The body’s ‘fight or flight’ stress response, which is designed to help us evade threats, also involves a sweat reflex. Stress-related sweat glands are concentrated in the armpits and groin, and tend to produce a thicker, fattier sweat than heat sweat.
Some people also find themselves sweating after a spicy meal. Capsaicin, the active ingredient in chilli, can fool the temperature sensitive nerves in the mouth into thinking that it’s hot, triggering a sweat response.
Why can the menopause lead to night sweats?
During the menopause, falling and fluctuating levels of oestrogen and progesterone can alter the sensitivity of the temperature-regulating centre in the brain. This is called the hypothalamus. And during menopause we can liken our hypothalamus to having a faulty thermostat. It means that we become more likely to switch on a vigorous cooling and sweat reflex, even in response to minor rises in temperature, or stressful situations.
When the hypothalamus switches on this vigorous cooling effort, we experience it as intense heat in the chest as the blood flow increases, spreading to the neck and face. Some women can experience dripping perspiration, while others may hardly sweat at all. During the day these episodes are known as hot flushes, and at night, night sweats. They typically last 1 to 5 minutes but can repeat 20 or 30 times every 24 hours.
We don’t yet know exactly why changing hormone levels impact on temperature regulation. But an overactive stress response, hypersensitivity of skin, or changes to metabolism may all contribute.
Are there other triggers for night sweats?
There are a wide range of other possible causes of night sweats, including infections, stress, alcohol, excess caffeine, low blood sugar and some cancers. Many women experience night sweats at certain times of their menstrual cycle, or during pregnancy. Certain medications, including some antidepressants, steroids and painkillers can have night sweats as a side effect. Chemotherapy and radiation therapy can also cause night sweats. There is also a harmless condition called hyperhidrosis that makes you sweat too much all the time.
So how can you improve your sleep when night sweats get in the way?
The faulty thermostat in menopause has hormonal origins, so if you’re struggling with night sweats speak to your doctor about whether hormone replacement therapy (HRT) could be suitable for you. Whether you are taking HRT or not, reducing exposure to triggers, and making it faster to cool down, can make the symptoms less intense, and make it easier to fall back to sleep.
Drink plenty of water during the day to help to improve temperature regulation.
Aim to keep your bedroom cooler than normal room temperature, around 19C. In summer, keeping the curtains drawn during the day, and keeping a window open at night could help if it’s not too noisy. Air conditioning might be helpful in extreme circumstances, but electric fans are a lot more energy efficient. Avoid the bedroom being cooler than 17C.
Choose light cotton pyjamas and bedding over less breathable materials. Pillows and mattresses designed with thermoregulating properties can be helpful.
If you’re sleeping with a partner, try separate covers. In warm weather, if you’re worried about night sweats, you might find that separate beds are better for your sleep.
Alcohol can dehydrate you and increases nocturnal sweating. Reducing or avoiding alcohol entirely can improve your sleep quality.
Regular physical activity is good for sleep quality and can also help to reduce hot flushes and night sweats. Choose a form of exercise you enjoy, so that you want to do it regularly. Low intensity exercise such as yoga and tai chi, strength based training and moderate intensity cardio have all been found to improve sleep quality.
Getting frustrated can make things worse. Remind yourself that night sweats are natural - it’s not your fault. Practice taking slow calming breaths to bring your heart rate down and help you to relax.
Keep a diary of your night sweats and hot flushes to see if you can spot any patterns. Were they related to feeling more stressed, smoking, or having caffeine, for example? Once you recognise your triggers it may be easier to manage them. A diary will also make it easier to check how effective interventions are.
Many of the tips which are true for sleep quality in general remain true if you’re suffering with night sweats during the menopause…
4 ways to sleep better during the menopause
The number one, evidence-based approach to treating insomnia, is called CBT-I or Cognitive Behavioural Therapy for Insomnia. This is a toolkit of different techniques which you try to help reinforce your natural sleep patterns and tackle negative sleep thoughts. Hormone Replacement Therapy may also help to reduce the frequency or intensity of hot flushes.
Here are 4 of the core ingredients of CBT which could be helpful to get your sleep back on track..
1. Get out of bed at the same time every day (even when you've had a poor night's sleep)
This anchors your body clocks, or circadian rhythm, and means you will automatically start to get sleepy at the same time each night. Your sleep is likely to be deeper after a short night of sleep to help you recover.
2. Take regular exercise
Secondly, regular exercise can help you fall asleep faster, and stay asleep for longer. As little as 30 minutes of moderate intensity exercise can help you sleep more deeply. If you’re not used to exercise, get help from an exercise specialist to gradually build up your strength and fitness.
3. Take time to unwind and detach from the day before bed
Thirdly, feeling stressed in the evening can interfere with the body’s natural production of melatonin. This can delay the body clock and lead to lighter, more disrupted sleep. Take time to unwind and detach from the day before bed. Relaxation techniques such as progressive muscle relaxation, yoga and mindfulness can all help switch off the stress response, and lead to more restorative sleep.
4. Only go to bed when you’re tired
Finally, only go to bed when you’re sleepy tired: the longer we stay awake, the more pressure to sleep we build up. If you don’t feel tired, do something relaxing until your eyelids feel heavy, and only then get into bed. If you’re feeling fatigued, a short 20 minute nap after lunch can be a useful boost to mood and energy levels







